Nurse's Notes : a Guide with Template
Get the work done for any meeting
Meeting transcription, AI custom notes, CRM/ATS integration, and more
You’ve just checked vitals, updated charts, comforted a patient, and handed off medication — but before you can leave, there’s still one task waiting: your nurse’s notes.
Done right, they make your job easier, not harder.
In this article, you’ll learn everything you need to write clear, professional nurse’s notes.
What are Nurse’s Notes and Why You Should Always Do One
Nurse’s notes are narrative entries that record what nurses do, what they observe, how patients respond, and what follow-up is required. These notes sit within the broader patient chart/documentation but focus specifically on the nursing care episode and the nursing process: assessment, intervention, and evaluation.
1. Continuity of care & communication
Patients may be attended by different nurses, shifts, or care teams. Clear nurse’s notes provide the next nurse with what happened, how the patient responded, and what to watch. Documentation supports hand-over and seamless care transitions.
2. Legal, professional & regulatory obligations
Your nurse’s notes are part of the legal medical record. They show what care was delivered, when and by whom — which is essential for audits, liability review, and accreditation. In fact, documentation errors or omissions are tied to many liability claims.
3. Monitoring changes & ensuring patient safety
Nurse’s notes capture changes in patient condition, responses to treatments, vital signs, and incidents. Good documentation helps identify deterioration earlier and supports safe, evidence-based decisions.
4. Supporting quality improvement & care planning
Well-written notes feed into care plans, audits, research and institutional quality improvement. They give insight into what’s working, what isn’t, and how care needs to evolve.
5. Protecting you professionally
For you as a nurse, comprehensive, clear notes defend your professional role: they demonstrate your assessment, your interventions, and your judgment. Poor documentation might not only inconvenience the team, but also place your license or liability at risk.
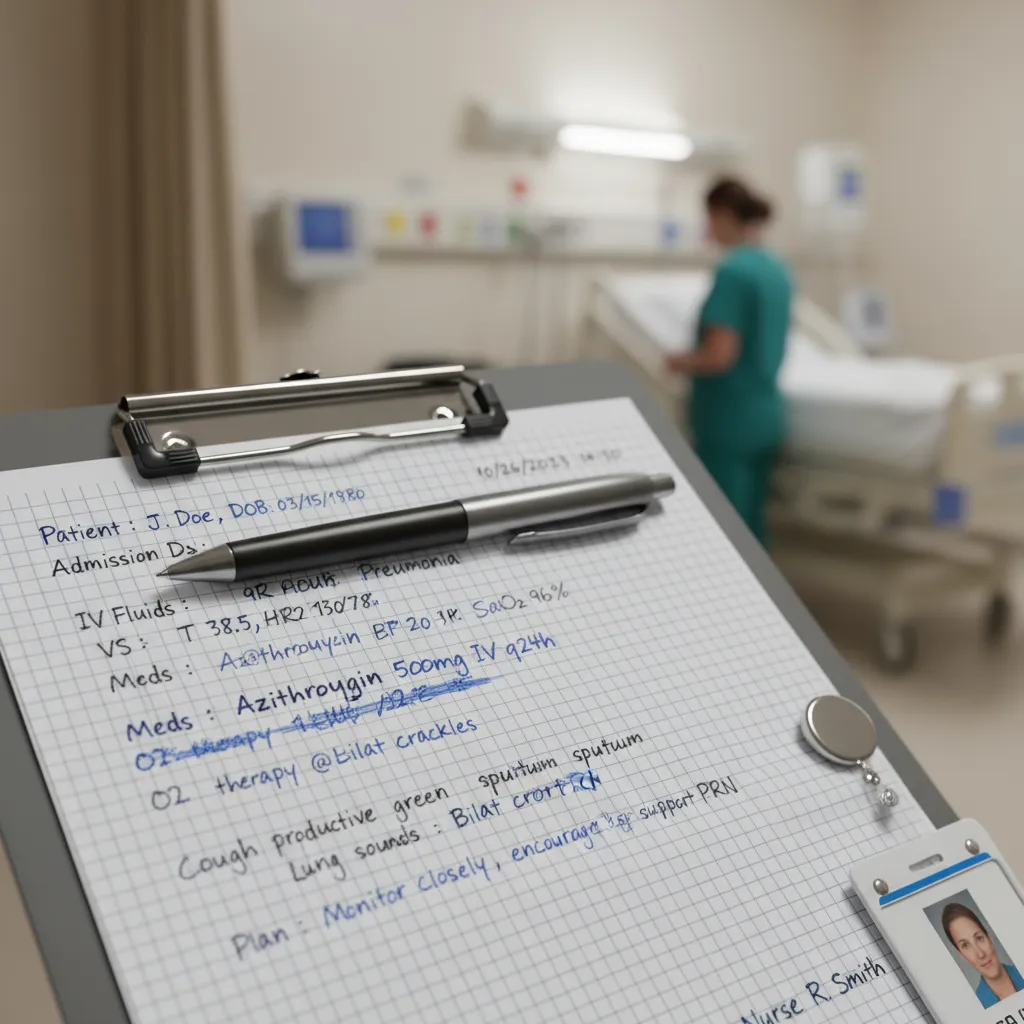
Structure & Example of Nurse’s Notes
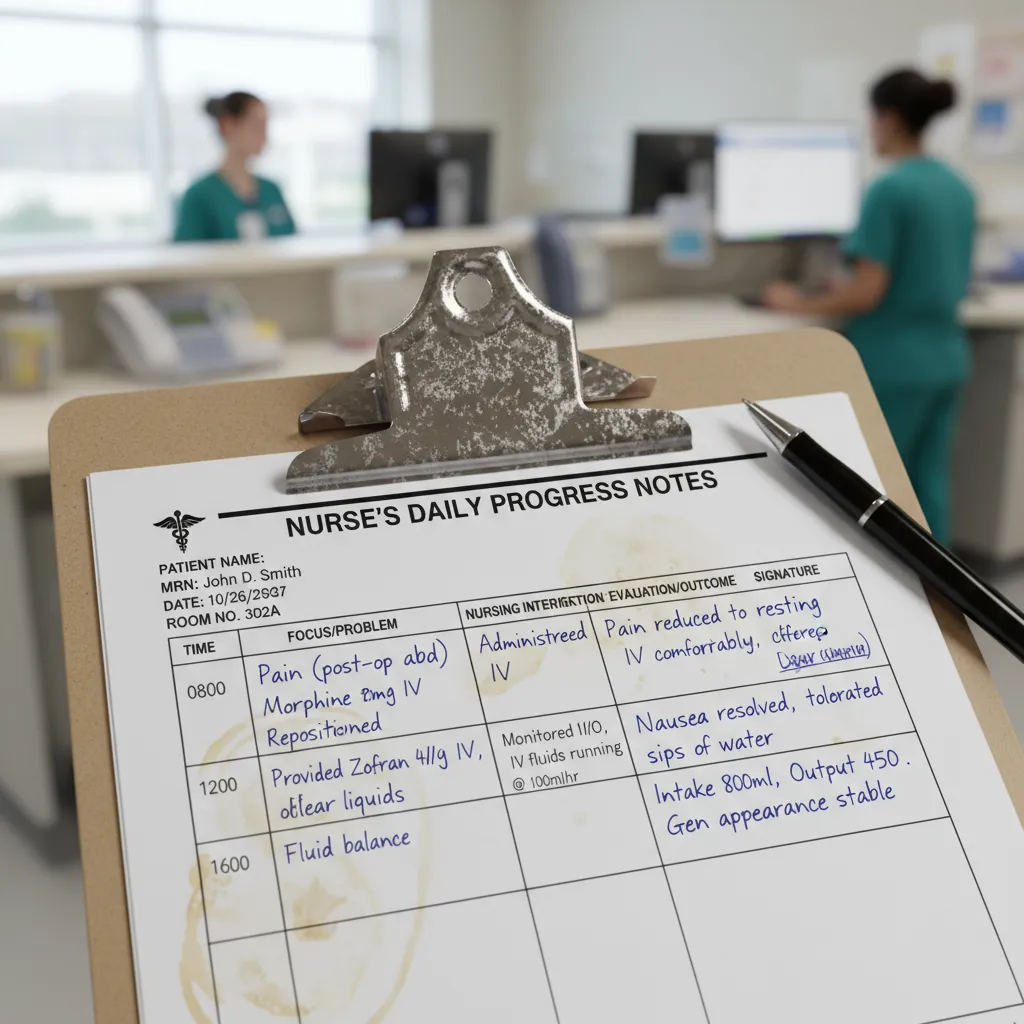
Every note you write should at minimum cover these essential elements:
- Date and time, patient name and ID, nurse’s name and credentials. Without those, the note lacks proper identification.
- Subjective data – what the patient says (e.g., “I feel chest pain,” “I can’t sleep”). If you record the patient’s own words, put them in quotation marks.
- Objective data – your assessment, vital signs, observable findings (e.g., BP 140/90, RR 22, wound size 4×6cm).
- Assessment/Analysis – your professional interpretation: what the issue is, changes you’ve noticed, clinical judgment.
- Intervention/Action – what you did: medication given, wound cleaned, referral made, patient education.
- Response/Evaluation – how the patient responded: did the pain reduce, did condition change, were there complications?
- Plan/Next steps – what will you (or the team) do next: monitoring, follow-up, adjust plan, refer.
Many institutions use standard formats such as SOAP (Subjective, Objective, Assessment, Plan) or DAR (Data, Action, Response) to keep things consistent and clear.
Strong example:
2025-10-26 14:30 | Patient: Mr Brown (ID A1234) | Nurse: J. Smith RN
Subjective: “My chest is tight and it’s harder to breathe than this morning.”
Objective: BP 150/92, HR 98, RR 24, SpO₂ 92% RA. Lung auscultation: bilateral wheeze, mild use of accessory muscles. No new edema.
Assessment: Suspected exacerbation of COPD, likely triggered by yesterday’s dust exposure.
Action: Administered salbutamol nebuliser ×2 doses per protocol. Educated patient on inhaler technique and environmental triggers. Notified MD and ordered ABG.
Response: After second nebuliser, SpO₂ rose to 95%, RR 20, patient reported “less tightness”.
Plan: Continue hourly respiratory obs, administer nebuliser every 4 hrs prn, review ABG results, alert respiratory team if no improvement by evening shift.
Weak example:
10/26 2:30 PM Mr Brown still struggling with breathing. Nebuliser given. Will watch.
Nurse’s Notes Template
Here’s a ready-to-use template you can copy, paste and personalise for your setting (hospital ward, clinic, home care, or long-term setting). Use it in your EMR, Word document, Google Doc or your preferred system — then tailor the fields to your facility’s standards.
Nurse’s Note
Date: _________ Time: _________
Patient Name: _________ Patient ID/Room: _________
Nurse Name & Credentials: _________ Unit/Area: _________
Subjective (S):
Patient reports: “_____________________________________________”
Additional comments: _______________________________________
Family/caregiver input: ___________________________________
Objective (O):
Vital signs: BP _____ / HR _____ / RR _____ / SpO₂ _____% / Temp _____°C
Physical assessment: _______________________________________
Relevant lab/imaging: _____________________________________
Medications administered: _________________________________
Other objective data: _____________________________________
Assessment (A):
Nurse analysis/clinical judgment: ___________________________
Nursing diagnosis or primary issue: _________________________
Intervention (I):
Actions taken during this shift/visit:
Patient/caregiver teaching or support: ______________________
Collaborations/referrals: __________________________________
Evaluation (E):
Patient’s response to intervention: __________________________
Changed status / new findings: ______________________________
If no response or adverse response: _________________________
Plan (P):
Next steps for nursing and care team: _______________________
Monitoring required (what parameter, frequency): _____________
Follow-up/referral details: _________________________________
Signature: ___________ RN/LPN Time: _______
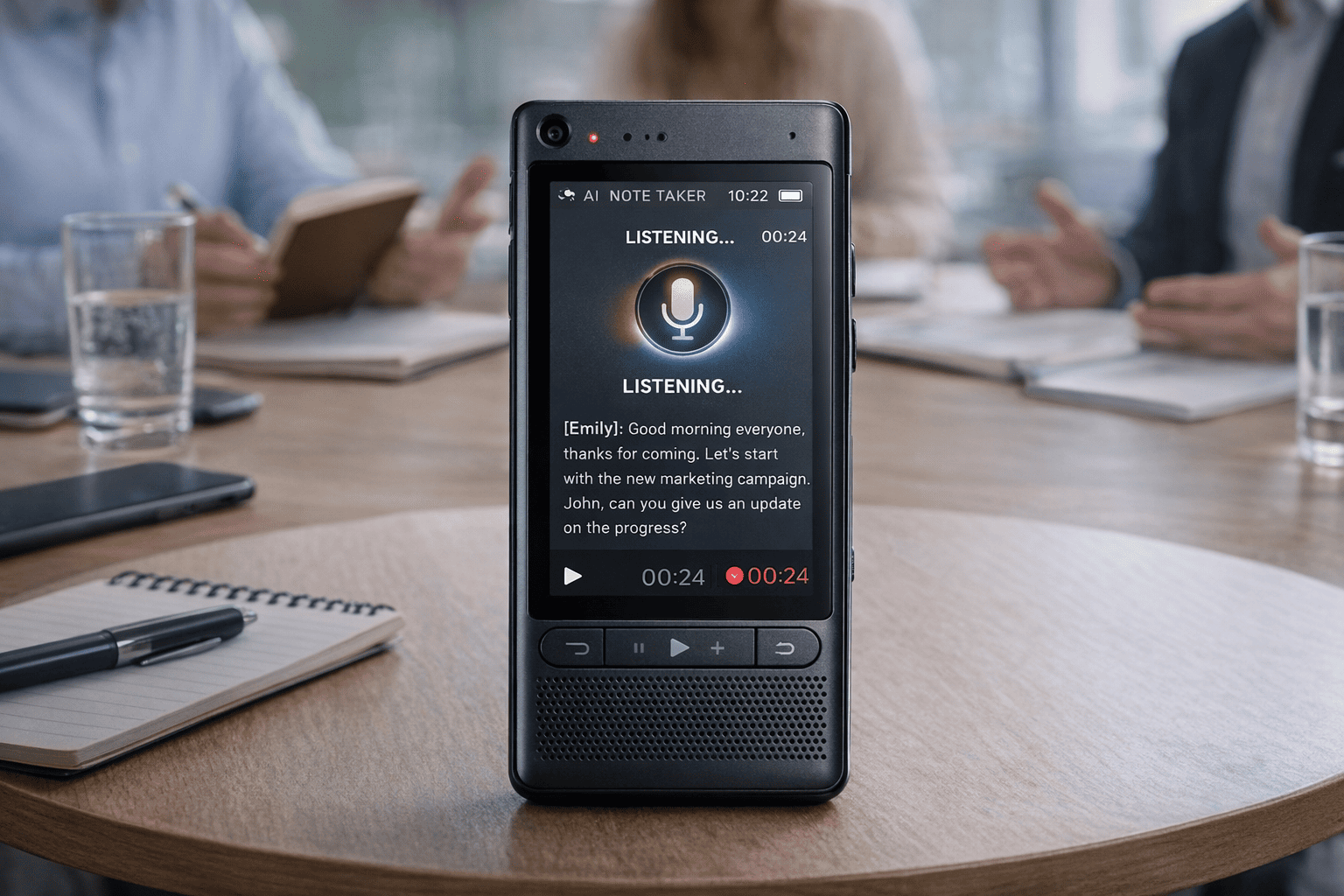
Automated Nurse’s Notes: Noota

What if instead you could automate much of that documentation, focus on the person in front of you, and still walk away with notes that meet your standard? Noota is a tool built with exactly that goal in mind.
- Records interactions, whether via video call or in-person meeting, and transcribes the audio in real time.
- Automatically generates structured summaries of those interactions—decisions, next steps, patient responses, key observations—so you don’t start from a blank page.
- Makes your notes searchable and archiveable. You’re not just producing text—you’re building a record that you (or your team) can query.
- Integrates into your workflow: you can link the output to your EHR, care-planning system or team hand-over process.
WANT TO AUTOMATE YOUR NOTE-TAKING BY RECORDING YOUR CONVERSATION ? TRY NOOTA FOR FREE NOW.
Get the work done for any meeting
Meeting transcription, AI custom notes, CRM/ATS integration, and more
Related articles

Forget note-taking and
try Noota now
FAQ
In the first case, you can directly activate recording as soon as you join a videoconference.
In the second case, you can add a bot to your videoconference, which will record everything.
Noota also enables you to translate your files into over 30 languages.

.svg)
.svg)

.webp)
.png)

.svg)
